The Veterans Affairs Community Care Program (VCCP) provides health care for veterans in need outside of VA facilities. A recent report exposed flaws in the Veterans Health Administration’s (VHA) ability to identify and exclude providers from the VCCP that have failed to deliver safe and appropriate care.
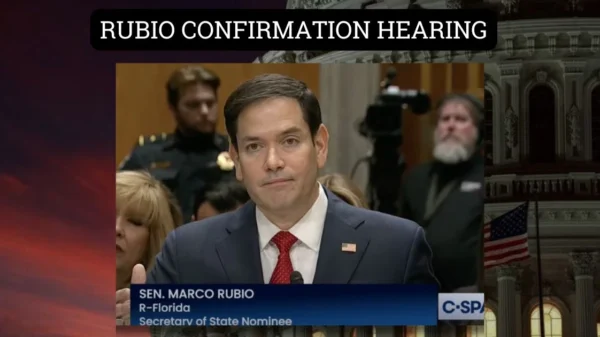
U.S. Senator Marco Rubio (R-FL) sent a letter to U.S. Department of Veterans Affairs Secretary Denis McDonough regarding the report and its impact on Florida’s veterans.
- “Veterans across the country deserve to know that when they are referred to a community care provider that the VA has ensured that the provider is one that will provide the safe, appropriate, reliable, and necessary care that the veteran deserves.”
The full text of the letter is below.
Dear Secretary McDonough:
I write out of concern following a recent report from the U.S. Department of Veterans Affairs (VA) Office of Inspector General (OIG) revealing that the Veterans Health Administration (VHA) failed to identify all healthcare providers that have been removed from VA employment due to violating policies related to the delivery of safe and appropriate care. The report further details that the VHA failed to exclude those providers from the VA Community Care Program (VCCP). Whether veterans receive care at a VA facility, or in the community through the VCCP, they are trusting the VA to refer them to qualified and reliable providers. I expect the VA to immediately implement the OIG’s recommendations and take further actions to rectify the VA’s processes that allowed such an oversight to happen in the first place.
The report stated that the OIG “remains concerned about VHA’s inability to exclude and prevent ineligible healthcare providers from delivering care to veterans through the VCCP.” The OIG discovered community care claims from healthcare providers that VHA had identified as ineligible to deliver such care. Further, the OIG found that the VHA failed to capture 81 percent of clinical occupations when identifying healthcare providers for exclusion due to violation of a policy relating to the delivery of safe and appropriate health care, according to the VA MISSION Act (P.L. 115-182). With an inability to identify providers that have previously violated care policies and, therefore, should have no role in furnishing care to veterans, the VA has no ability to exclude these providers from participating in the VCCP in the future.
While this is an issue that needs to be addressed nationwide, one specific instance the VA OIG has considered in recent months resulted from a case involving a surgeon who had a medical license revoked in Florida but later would participate as a provider in the VCCP. The OIG found that the surgeon voluntarily relinquished a Florida medical license after being investigated by the Florida Department of Health and notified of “a potential termination for cause.” The OIG stated that Optum was unclear on whether such an instance should be considered as part of the VCCP credentialing process, and OIG stated that the VA’s contracts do not address or define this terminology.
Unfortunately, the OIG’s recent reports are not novel assessments of the VA’s lack of ability to track the reliability of providers in VCCP. In 2021, the Government Accountability Office found that gaps in VHA’s ability to identify providers ineligible to participate in the VCCP. At the time, VHA assessed 800,000 providers and identified 1,600 VCCP providers “who were deceased, were ineligible to work with the federal government, or had revoked or suspended medical licenses.” As an example, one of the providers was convicted of patient abuse and neglect in July 2019, but entered the VCCP in November 2019 – to which the VHA stated the provider was uploaded in error. This is unacceptable.
Veterans across the country deserve to know that when they are referred to a community care provider that the VA has ensured that the provider is one that will provide the safe, appropriate, reliable, and necessary care that the veteran deserves. I would like to receive regular updates on VA’s plans to implement the OIG’s recommendations, and also request answers to the following questions:
- What steps are being taken to ensure that the reasons for healthcare providers’ removals are accurately documented and considered in the exclusion process?
- What improvements or updates to the process is the VA planning to implement to ensure that no eligible provider is wrongly excluded from the VCCP?
- How is the VA ensuring compliance with the MISSION Act section 108(a)(1), which required the VA to exclude VCCP eligibility if the healthcare provider was removed from Department employment, in their current operational procedures?
- How often does the VA periodically review the effectiveness of its exclusion processes?
- What specific measures are being implemented to include all clinical occupations in the automated query used for identifying providers for exclusion?
- How is the VA addressing the issue of incomplete coverage of personnel actions in the data that leads to missing out on identifying providers who should be excluded?
- How does the VA plan to inform patients when a provider has been excluded?
I appreciate your attention to this important matter.